
FORMATION AND SPREADING OF BIOFILMS
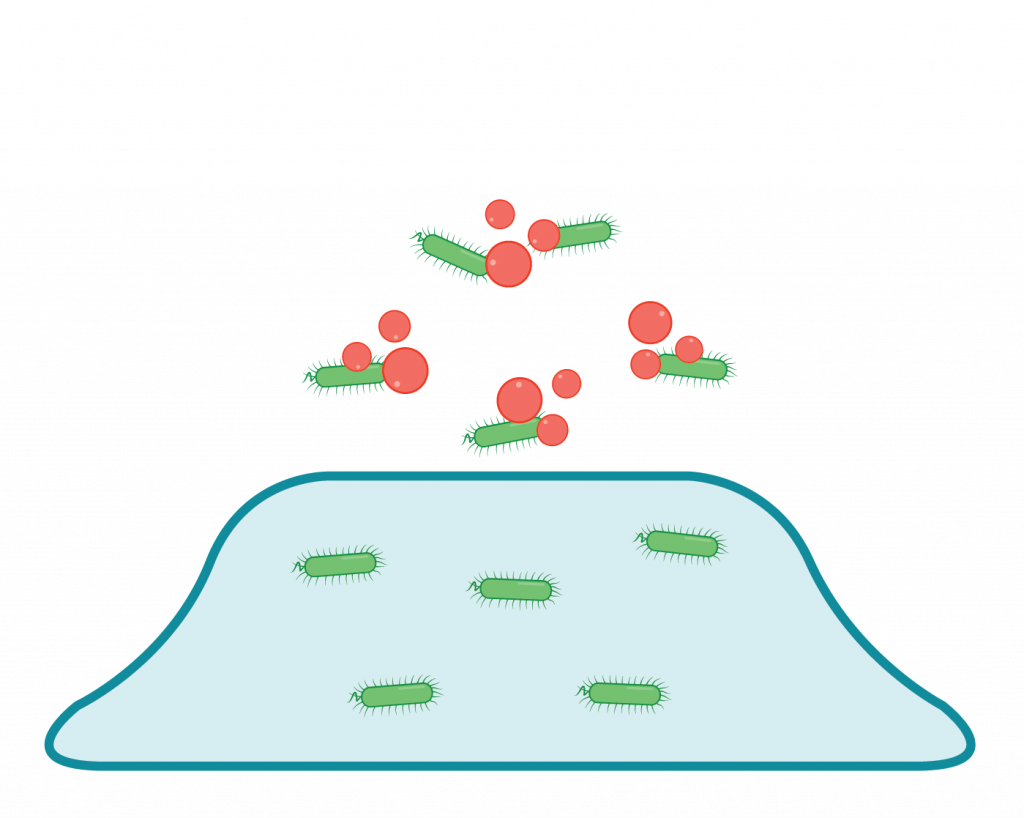
Biofilm development is well organized and during its development intercellular and intracellular signalling occurs. A panel of genes/proteins are upregulated as well as downregulated for attachments of bacteria onto host cells. Biofilm can be formed within 24 hours after attachment. There are five main steps for the formation and spreading of biofilms (see figure 2). After the attachment phase, the bacteria will start to form a (mono)layer and produce a polymeric matrix layer for protection. In the last stage, some cells or parts of the mature biofilm start to detach and disperse into the environment as planktonic cells again. They can start a new cycle of biofilm formation elsewhere in the body (Guzmán-Soto et al., 2021).

Figure 1: Schematic representation for single bacterial species biofilm formation on a solid surface (AHV International, based on Guzmán-Soto et al., 2021)
BIOFILMS AND THE HOST IMMUNE SYSTEM
In short, biofilm formation is a survival strategy or defence mechanism for bacteria. It is highly difficult to eradicate biofilm using the available variety of commonly known/used instruments, while the animal’s immune system cannot detect and phagocytose the bacteria inside a biofilm (Prakash et al., 2003).
Initial infection
Bacteria invade the host causing infection and form an extracellular structure – biofilm

Dormant period
Biofilm “protects” the bacteria inside as it is impenetrable to antibiotics and immune cells

Chronic infection
Upon reaching sufficient population, bacteria in biofilm reoccur in planktonic state and cause recurring infections
Figure 2:
This means that the animals’ immune system is only triggered by planktonic bacteria and not by bacteria hidden in the biofilm. In situations involving all kinds of stressors, the animals’ immune system will become suppressed. Then there is a risk that bacteria from the biofilm will become planktonic, which will lead to new challenges (see figure 2).

Figure 3: Recurrence of chronic infections by immune suppression in combination with biofilm formation
Chronic biofilm forming issues can be observed in Dairy cows; Streptococcus dysgalactiae, Streptococcus agalactiae, Streptococcus uberis and Escherichia coli (M.B. Melchior et al., 2006). Swine: Streptococcus Suis (Yang Wang et al., 2018. Clostridium perfringens (A. (Charlebois et al 2014). Avian Escherichia coli (APEC) (Kushal Grakh et al 2022). To keep animals healthy, biofilm formation must be prevented.
BIOFILM IN RELATION TO ANTIMICROBIAL RESISTANCE (AMR) DEVELOPMENT:
Because of the dense polymeric matrix of biofilms, antibiotics penetration will be limited, with the result that a gradient will be formed under the bactericidal critical level, resulting in faster development of microbial resistance (Philip S. Stewart et al., 2002 / Niels Høiby et al., 2009). These subinhibitory concentrations of many antibiotics are able to enhance biofilm formation by pathogens (Kaplan, 2011). Therefore, approximately 80% of chronic and recurrent microbial infections in the body are due to bacterial biofilm. Microbial cells within biofilms have shown to be 10–1,000 times more antibiotic resistant than the planktonic cells (Abranches J., 2011).



